🦀 Issue 122 - IT Problems. Let’s Reboot It.
This week on PT Crab we’re going back. Back into some info we’ve seen before to build a more summative picture of what we know. And an even more summative picture of what we don’t. Because this week we’re looking at IT band pain. It’s a retrospective followed by a summary followed by the possibility of increased confusion but hopefully some clarity. And speaking of confusion, you should know before we start that the reliability and validity of the two most common ITBS tests aren’t known. Noble’s Test and Renne’s Test? Maybe amazingly useful. Possibly impossibly useless. No data to date. Ick.
But it’s not all confusion and lack of data, there is some stuff that we know. So let’s look at we know, speculate on what we don’t, and think about where to go from here.
P.S. Because I’ve gotten some questions about it recently, PT Crab stands for Physical Therapy Clinical Research, Awesomely Brief. Jsyk. Which stands for just so you know, just so you know.
P.P.S. You’ll notice that this edition is really long. It’s what the supporters get every week and they support the Crab for about $1 per issue. You can get this much content every week by upgrading your subscription here.
Let’s dive in!
We Don’t Know ITBS
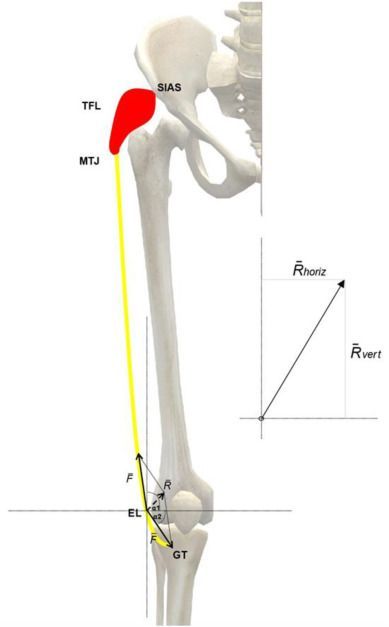
The Gist - Everything you know about treating ITBS could be wrong. Or it could be right. The truth is, we don’t really know, at least according to this Austro-Spanish (I wonder if that empire would’ve been broken up as easily as the Hungarians…) team publishing in Physical Therapy in Sport. They dive into a mathematical model to discuss pathogenic factors of IT band syndrome then take a second dive (a real Tom Daley move, without the knitting) to see what we know about treating it. Their mathy model explores the physical expectations of IT band pain and predicts some remedies that their dive into the literature doesn’t bear out. Overall, a really interesting piece.
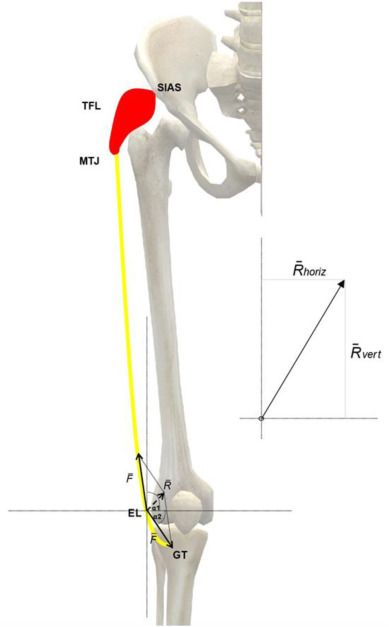
But what did they actually say? Well. First off, according to a study they cite from 2013, only 44% of people recover from ITBS during 8 weeks of therapy. So this is an important area. The semi-systematic review they did reveals that soft tissue techniques are theoretically plausible but the research on them is limited so far. Hip strengthening is also plausible and has been demonstrated to be effective, but little pure strength research has been done. And lastly, stretching of the glute med, TFL, and glute max has shown some transient effects and are theoretically plausible, but we don’t know. So… yea.
As far as the causal speculation goes, there’s more than just this, but it’s pretty well summed up here along with associated citations.
As an example, knee varus and internal rotation shift Gerdy's tubercle in the medial direction, which increases ITB strain (Baker et al., 2018; Ferber et al., 2010; Hamill et al., 2008; Kim et al., 2020; Meardon et al., 2012; Stickley et al., 2018). Such tensioning might limit the tendon's capacity to dampen force peaks by storing elastic energy. Although studies providing robust mechanistic explanations are missing, cross-sectional studies comparing the running kinematics indeed suggest that during the stance phase the peak hip adduction and knee internal rotation are greater in runners with ITBS (or those who go on to developing the syndrome) as compared to healthy controls (Mousavi et al., 2019). Consistent with these observations, several studies found hip abductor weakness to be associated with ITBS, although the notion is not undisputed (Mucha et al., 2017). Improper lower limb alignments at the ankle or foot, such as increased rearfoot eversion (Balachandar et al., 2019), might coincide with malalignments and increased stresses at the knee, although further research is required to confirm the role of ankle or foot malpositions in the etiology of ITBS (Ferber et al., 2010; Noehren et al., 2007; Suárez Luginick et al., 2018).
Yea, it a lot.
Tell Me More - Lastly for interventions, they looked into running retraining. This is gait retraining separate from muscle strengthening, kapeesh? But there’s very little data to back it up so far. So we don’t really know.
So what have we learned today? It’s that we don’t know. We do know that a lot of our work on ITBS is based on tradition and expert opinion and that we need to do more work. We also know that these authors have a significant bias toward a pathoanatomical process of pain and give very limited shrift to a more complex biopsychosocial one. I know that ITBS isn’t chronic low back pain, but that doesn’t mean there’s not room for a BPS approach. And the more we learn about the body, the more we know that pain doesn’t necessarily line up with dysfunction. It’s annoying, but true.
What this paper does well is process through the clinical reasoning behind ITBS and posit possible solutions while backing them up with the relatively limited amount of evidence we do have. It’s a good read, all things considered.
And if you’re interested in an even deeper dive into ITBS, including our (mostly) complete history of how we’ve treated it, see keep on going.
That was long, are you done now? Yes. Here’s the paper.
IT History.
The Gist - This fantastic summary by an ATC, Paul Geisler, breaks down the complete history of ITBPS, including the current view of what causes the pain and how to fix it in a slightly different way than the paper above. The history section is incredibly interesting, starting with a description of the IT Band’s first discovery in 1843 and taking us through the entire pathohistorical pathway to understanding ITBPS. But I’m just gonna start with today’s deets, since that’s probably why you’re here. But seriously check it out for the history, it’s great.
According to this paper, our current, evidence informed model of ITBPS says that the Ober test does not demonstrate a tight IT band, since the IT doesn’t limit adduction (glute med and min do) and that the IT band cannot be stretched. Even stretching TFL doesn’t help because of the IT’s multiple attachments to lower fascial and bone layers that have been discovered over the years. Nor does the IT band roll over the femoral condyles, for the same reason (which is probably why the Noble’s and Renne’s tests possibly don’t really work). Rather, the cause of IT Band Pain Syndrome is related to impaired hip musculature that allows femoral drift into the frontal plane in running, leading to femoral adduction and internal rotation that causes sub-IT fat pad impingement. Probably. And since the causes took that much room, let’s go to the next session for assessment and treatment.
Tell Me More - Assessment is recommended to be a thorough history that includes recent changes in training volume or any hill running (especially downhill) and both history and (possibly) palpation that demonstrate sharp, focal lateral knee pain. You can also have the person jog for about 20 minutes on a treadmill and watch for femoral adduction at the end, during the stance phase, demonstrating lack of hip control. For people who are used to running longer distances, you may have to get them to run a longer distance before their abductors get tuckered out, so clear your schedule it you’re treating an ultra runner.
Treatment? The author goes through three levels of management, so I won’t dive into all, but here’s the gist of each one:
- 1 - Low-load, open chain phase focusing on motion control in hip exercises
- 2 - Moderate-load, closed chain phase focused on keeping pain low, increasing endurance, and training hip control
- 3 - High impact, tolerance, and ready phase focussed on sagittal plane control, landing drills, flat ground running, and more
I highly recommend reading the whole paper. So, do that.
Paper? Yupp. Read it.
IT Bands Are Backward
The Gist - O.o - That about sums up this juicy bit of research from the Journal of Physical Therapy in Sport. Researchers from Austria used a new type of ultrasound, shear wave elastography, to figure out what IT band tone looks like in runners with IT Band Syndrome and compare it to non-runners and themselves after treatment for their problems. Pre-treatment, there were no differences detected between the IT band characteristics and hip muscle strength between the injured runners and healthy controls. The injured went through a 2 week period of manual therapy followed by 4 weeks of neuromuscular education, strengthening exercises of their hips and stretching and foam rolling of their IT bands, glutes, and TFLs. After all this, the runners got way better (average pain down from 7.8 (ow!) to 1.7), but their IT bands got stiffer, not longer and more flexible like the researchers predicted. Weird.
Tell Me More - This requires elucidation, I know. According to the paper (and the others that you’ve already read), the major theory behind ITBS is that it’s an impingement syndrome caused by cysts, bursae, or fat pads underneath the IT band being compressed by a hypertonic band, causing inflammation and pain. That’s why the researchers tried to measure IT band tension before and after rehab. Even though these patients got way better (down 6.1 pain points, up 17% on the LEFS, and 50% reported being pain free), their IT bands got stiffer. According to the standard theory, they should have felt worse. Weird. This throws a shadow over that theory, though it’s not too dark a shadow yet. Things are still early. Here’s why:
- The study was only 14 people. Yea, not great.
- The runners were told not to run for 6 weeks which could have prevented inflammation from the IT band rubbing around down there.
- Shear wave elastography is still young and we’re not sure of its test-retest reliability yet.
Still, this is new, interesting information and I hope the researchers expand this study in the future.
Papel señor. Seguramente.
So what have we learned today? ¯\_(ツ)_/¯
Like I said above, ITBS is complicated and we’re not really sure what’s going on. I hope reading these three papers has given you some idea of what we’re actually dealing with. My goal is to make you look critically at your treatment, the wheres and whyfores, to determine if there’s something different you could be doing or a different way you could explain things to your patients. I hope to have done so.
To those who like treating ITBS, what do you do and how well does it work? I’d love to hear some opinions and theories.
Also, sorry I’m late, this week was nuts. But we made it.
Best,
Luke
