🦀 Issue 149 - Stuff we kinda don’t know
This week’s papers are about things that we’re not really certain about. I spend a lot of time discussing what we know, so instead let’s talk about what we kind of know, but not really. Today’s batch of things are SIJ pain provocation tests, running shoe prescription, and who would benefit from having aerobic exercise added to neck pain treatment. And that’s it, that’s all I’ve got.
Anyway, let’s dive in!
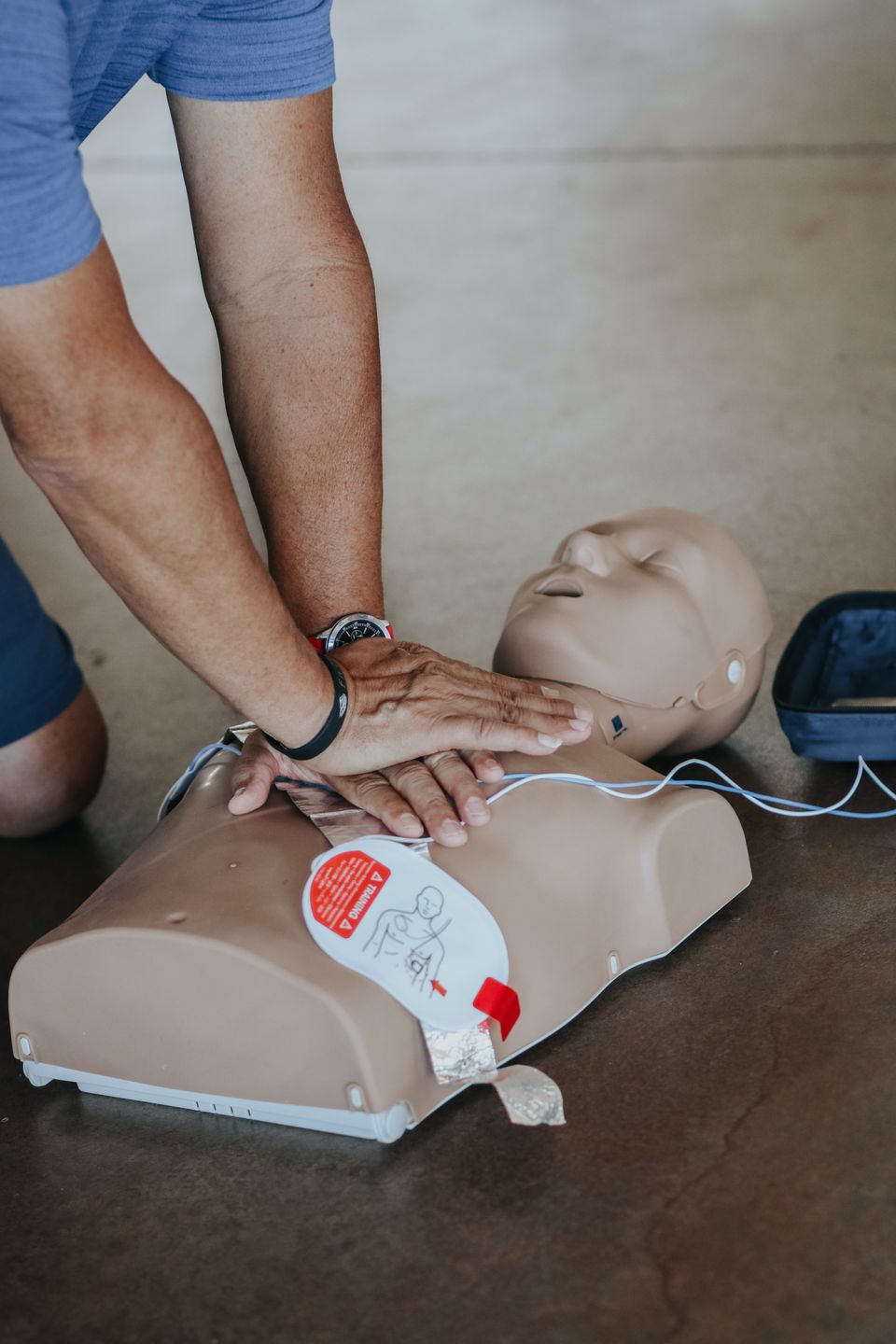
CPR for Necks
The Gist - That’s CPR as in - Clinical Prediction Rule - you know, like that one you’ve heard of for who would benefit from a lumbar manipulation but you don’t really know any other ones. Well these researchers attempted to come up with another one, doing a secondary analysis of a study from a few years back to see who would benefit from the addition of aerobic exercise to neck pain treatment. If you’ve been here before (which, let’s face it, you have), you’ve probably heard me talk about how a return to normal activity and aerobic exercise can be a big help for whiplash and neck pain in general. And while that’s true, it’s not true for every single patient. These researchers wanted to know for whom it was good, so they did.
They reanalyzed a previous RCT that included 139 patients, 62 of which were in the aerobic exercise plus neck PT group. Not everyone in that group improved, but many did, so they looked into who those people were. Those who did improve were consistent across 3 factors: 1) neck pain duration was less than 6 months, 2) Neck flexor endurance test result was greater than or equal to 18 seconds at the beginning, and 3) they were experiencing no referred pain.
Now, this result was disappointing, for me. Because I originally came across this paper in searching for interventions for a patient who matches exactly none of these criteria. But hey, we can’t all win. The researchers stress that it’s too early to call this a clinical prediction rule and they’re right. It requires validation. But it’s the first step into a larger world that you need and it’s also something that you could try out.
Tell Me More - But wait, you ask (which is weird, because “wait” Isn’t really a question). What about the parameters of the interventions that were actually used? (Ah, now that is a question) Well, here’s what they were.
Stretching of the UT, anterior and medial scalenes, pec major, and sub occipital muscles. Strengthening of cervical extension and flexion, shoulder protraction, seated rows, shoulder elevation in scaption, and horizontal abduction with ER. Those were the exercises that both groups in the initial RCT got. As far as aerobics went, they were given moderate cycling, at 60% of age-predicted HRmax. For the first week, that was 20 minutes at a time, 2 days per week. For the second, 30 minutes, and the third through sixth, 45 minutes.
Outcome measures were taken at baseline, 6 weeks (the end of the initial intervention) and 6 months. These were pain, the NDI, the FABQ, the Global Rating of Change (GROC) scale, and whether or not patients were experiencing cervicogenic headaches.
If you want all the math behind the decisions and analysis they made and did, read a different newsletter (and tell me about it because I’m a nerd and it sounds cool). What I’m going to close with is the end of this paper
It is worth noting that the CPRs of this study indicate that this kind of treatment program is not of much benefit to patients with persistent NP, only to those with NP that has lasted <6 months, with a NFE hold time >18 seconds (the mean NFE for patients with NP is 24.1 seconds),44 and no referred pain. Thus, patients with persistent NP and serious NP disorders need more involved therapeutic intervention, not just exercise training.
Just keep that in mind, k?
Paper? Right here folks.
We really don’t know anything about shoes
The Gist - Running shoes, that is. I mean, they look cool. But that’s just expert opinion (I’m an expert on cool, didn’t you know that?) and expert opinion is the vast majority of what we know about running shoes. This excellent piece in the Journal of Athletic Training really points that out. Sure it’s from 2020, but unless the pandemic was as big a revolution in shoe research as it was in my ability to waste time on the internet, we haven’t made it too far.
We do know that injury frequency has remained essentially constant as running shoes have evolved, but that doesn’t really tell us anything because it’s not stratified by experience or distance. We do know that (mostly) the MSK system prefers a specific movement path and will make subtle adjustments to maintain that regardless of shoe choice. Fun fact while we’re talking about what we don’t know, there isn’t a good way to predict running injury, including drastic increases in training load. Tell that to my swollen knee. (I do have a knee injury, but it’s weird and minor and strangely complicated and we’re not going to get into it but it doesn’t hurt when I’m running so I keep doing that because I’m a runner and we’re insufferable like that)
And that’s our week folks. Thanks as always for being a subscriber and do enjoy your weekend. Please invite your friends and coworkers. Forward this like it’s a 2004 chain email that promises your mom will die if you don’t. Because she will.
Bye!






Comments
Want to leave a comment and discuss this with your fellow PTs? Join PT Crab and get summarized PT research in your inbox, every week.