PT Crab 🦀 Issue 169 - Best of Foot and Ankle

It’s almost time for new content, that will first start appearing with issue 171. We’ll start out with a deep dive into the Chronic Pain Scale, a relatively new approach to pain measurement that could help you work with patients with chronic pain. After that, we’ll be looking at if meniscectomies work at all and how to help your patients after them. Then we’re going into strategies to treat adults with autism as an outpatient PT, and how you can use the concept of Joint Position Sense to improve your practice.
If you find those interesting, become a supporter for full details. The free edition will have one paper on each, while the supporters edition will feature three, plus summative education to help you use the information inside. I’m trying to make the research more actionable for you so you can finish an edition and change your practice that very day.
That’s then, this is now.
If you want to help the Crab out, there are three easy ways today:
Fill out the survey - I’ve learned a lot about y’all and would love for some more info. It’s just a few questions and it’s here.
Make a One Time Donation - Don’t want to pay $5 per month? How about just a buck or two every once in a while? If the Crab has been helpful for you and you want to, you can buy me a coffee here.
Tell anyone about the Crab - I’ve started advertising a tiny bit, but all new subscribers come from satisfied ones like you. So tell anyone. Forward this now! If everyone in your office isn’t a subscriber, I blame you. Yes. You.
With all that out of the way, let’s dive in!
When to Lift the Heel
The Gist - This brief piece on foot orthoses for scoliosis looks at 8 papers from the last 30 years assessing heel lifts to help people with scoliosis. The authors posit that leg length discrepancies and scoliosis aren’t well-associated yet, though their research points to it. The results of their review also back up the use of heel lifts to assist with the reduction of scoliotic curves. The functional leg length discrepancy appears to be on the concave side of lumbar scoliosis and doesn’t seem to be associated with thoracic curvature. In addition to the pelvic rotation in the frontal plane, an anterior-posterior pelvic rotation also commonly exists, as does one in the transverse plane. Basically, it’s all twisted up in there.
But a heel lift may help! We don’t have as much data on this as the authors would like, but lifts definitely help in functional scoliosis, with multiple papers pointing this out, including one with 369 people aged 5-17. The correction of leg length discrepancies in these people reduced scoliotic curves immediately and kept it up 8-16 months later.
Tell Me More - There’s not a ton more to tell in this short piece unfortunately. And I’ll be honest here, I don’t really like the piece. Sure, it gives us some info, but it’s empty, non-specific, and doesn’t really change much. I’m actually sorry I picked it, but by the time I reached this conclusion I was pretty far down the road of reading it and breaking it down and it’s just to late to change, okay? Sorry about that. I’ll make it up to you by recommending you listen to St. Paul and the Broken Bones. They’re an excellent band and I especially recommend All I Ever Wonder and this album recorded at SXSW in 2014 and featuring Lizzo. Does this help your practice? Yes. Cuz you’ll be happier, so you’ll practice better. Duh.
Paper? If you must. At least it’s open access.
Navicular Drop Test. It’s Easy and It Works
The Gist - Researchers wanted to see how the quick and easy navicular drop test compared to the Foot Posture Index and footprint parameters, so they grabbed 71 people and did some calculating. The navicular drop test is a simple way to evaluate the medial longitudinal arch of the foot. The researchers argue that that’s important, since:
A decrease in the MLA height is related to modifications in the lower limb alignment, including subtalar pronation, tibial internal torsion, tibial internal rotation, greater genu recurvatum, anterior knee laxity, pelvic anteversion, and lumbar lordosis. The height of the MLA may affect muscular activity. A Navicular Drop Test (NDT) score of ≥13 mm is associated with decreased concentric plantar flexion strength compared to normal MLA. In addition, the height of the MLA is considered a relevant factor for several lower limb pathologies, including medial tibial stress syndrome, patellofemoral syndrome, and non-contact anterior cruciate ligament injuries and foot pain.
So yeah, it’s a big deal.
To pull off the NDT, the patient stands barefoot, you mark their navicular tuberosity, palpate the lateral and medial aspects of the taller dome, then move the foot until the talus is centered. Lastly, you measure the distance from the navicular tuberosity to the floor. On this test, interrater and intrarater reliability were excellent (>.9) and correlation with the FPI and footprint measurements were very high as well. Great news for the test.
Tell Me More - This was only tested in people with a low medial longitudinal arch, so it may not be generalizable to a full population, but it’s still great news for an easy test. The researchers argue that this measurement is essential in foot and lower limb assessment since it’s so closely related to so many conditions. Keep in mind that this doesn’t necessarily mean a big navicular drop causes those conditions, it’s just an association. Now that this test shows great reliability, it makes navicular drop much easier to measure in a clinical scenario. It should take under a minute to pull off. Yay!
Paper? Of course dood. Open access here.
Crossfit for Chonic Ankle Instability. Workout of the Day the Pain Away.
The Gist - These athletic trainers from Spain and Miami found 70 recreational athletes with Chronic Ankle Instability and randomized them into three groups. One took on CrossFit training alone, performing an organized workout that included elements of mobility and power. The other carried out the same CrossFit workout, but did ankle self-mobilizations first, then did some CrossFit. The other other group was the control, so they did nothing. The CrossFitters worked 2x/wk for 12 weeks.
Outcome-measure wise, they looking at Ankle-dorsiflexion range, subjective instability, and dynamic postural control using three different tests.
Afterward, those who performed the self-mobilizations improved most across all outcome measures while those who just performed CrossFit improved quite a bit. The control group did not improve. Self-mobilization was better than just CrossFit across all outcome measures except the CAIT, a questionnaire that assesses the severity of ankle instability. This piece really shows that motion is indeed lotion and focused motion is the best lotion.
Tell Me More - All groups started with about 8.7° of ankle dorsiflexion range and the self-mobilization folks increased that by 2.29° while the CrossFitters increased it by 1.6°. On the CAIT, self-mobilizers improved by 5 points (going from 18.8 to 24.16 on a scale where >25 indicates no chronic instability) and CrossFitters improved by 4.4 points (18.9 to 23.3). On the individual level, in dorsiflexion range, 56% of the mobilizers had changes that broke the MDC barrier which is great news.
All of the mobilizations they used were weight-bearing and referred to as “Mulligan-type”, AKA Mobilizations with Movement. They included a lunge with a kettlebell over the forward knee and max dorsiflexion, a talo-crural distraction with band and then passive dorsiflexion with another band, and talar posterior mobilization with a band while actively dorsiflexing. If my descriptions don’t cut it, the article has photos.
The best news was the improvement on the CAIT in both groups. According to the researchers, “Another important aspect of patients with CAI is the self-reported feeling of instability…. The improvements of 96% and 83% of the participants in the self-mobilization plus CrossFit and CrossFit-alone groups, respectively, can be considered the greatest strength of the present study.” And I agree.
Paper? Sure thing.
Cuboid Syndrome Apparently Exists
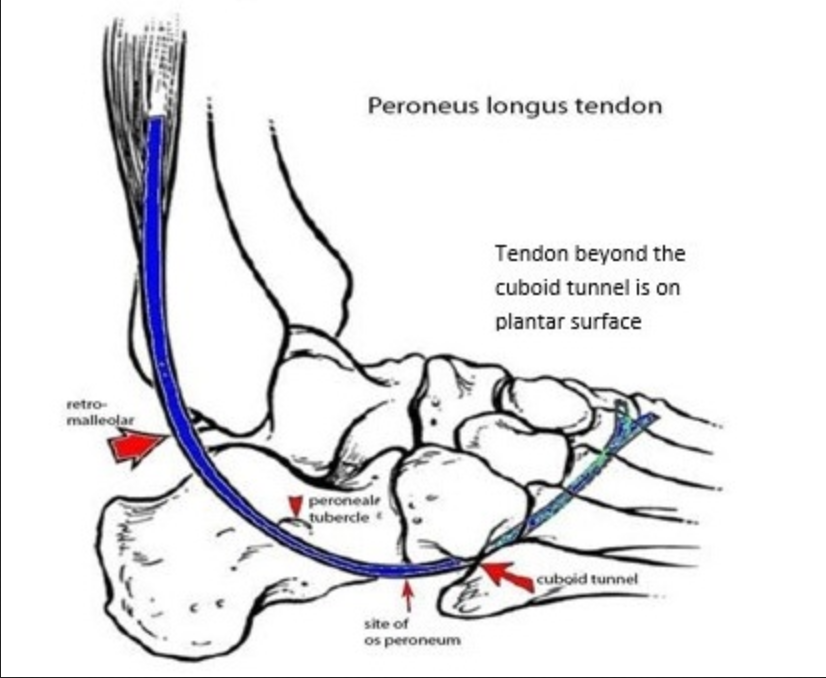
The Whole - This literature review from the journal Sport Physical Therapy (and from 2011) is about Cuboid Syndrome, an interesting condition that I thought I’d highlight because I have it. If you want information about your own conditions, write your own newsletter! (But actually, if you want information about anything in particular, email me and I’ll get it in a future Crab. Or just start your own newsletter, it’s fun. Sometimes.) Cuboid syndrome, according to the paper, “is an easily misdiagnosed source of lateral midfoot pain, and is believed to arise from a subtle disruption of the arthrokinematics or structural congruity of the calcaneocuboid.” It most commonly occurs along with a lateral ankle sprain, but can develop chronically in athletes, usually dancers. Basically, this super stable joint gets unstabled by the fibularis longus tendon yanking it out of position. The tendon loops under the cuboid (see the photo, it cleans things up in your head)
and chronic uncontrolled pronation can pop it out of place. Unfortunately and fortunately, this out-of-placeness is very minor, so much so that it can’t be seen on radiographs.
How do we know it’s messed up then? Tests my dear Watson. There are quite a few things that can cause lateral foot pain, as I’m sure you know, so you have to screen those out as best you can. Fortunately, the best way to diagnose it is by treating it. If the manipulation for it works (the cuboid whip), then it’s probably cuboid syndrome. Padding under the cuboid to help it from wiggling around is handy too.
The paper has a fair bit more about this if I’ve piqued your interest. It’s an under-studied topic but I can direct you to more about it if you want was well. Just lmk!
Paper? Indeedy-doody.
And that’s our week! If your desk buddy still isn’t subscribing remember, it’s your fault. So fix it now. And goodbye!






Comments
Want to leave a comment and discuss this with your fellow PTs? Join PT Crab and get summarized PT research in your inbox, every week.