Issue 32 - The Controversy Issue
We’re back to our eclectic selves at PT Crab, with this week’s articles featuring the risk factors for pelvic girdle postpartum pain (and they’re not what you’d think. Okay, maybe they are…) and a new tool to evaluate shoulder instability risk. Could a questionnaire really show if you’ll dislocate your shoulder again next year? The PRIS tool thinks so.
Want to read a controversial take about pre-treatment positional testing of the vertebral artery and learn about how to better prescribe exercises for FAI? Then make sure you get down to the bottom of this edition. And thanks for being a supporter! Only King Crab members get those two articles and you are part of the lucky ones. Thanks!
Here we go!
Are You At Risk for Pelvic Girdle Pain? Probably not. But Your Patient May Be.
The Gist - Pelvic PT is growing rapidly, and that’s awesome. If you’re a pelvic health therapist, here’s some interesting stuff for you! And if you’re not, it’s still interesting, since it’s about the risk factors for postpartum pelvic girdle pain. If you’ve ever treated or will ever treat someone who’s pregnant, read on MacDuff.
It’s a big systematic review and meta-analysis, so I’m just going to summarize the most significant risk factors for postpartum pelvic girdle pain here:
- Pelvic Girdle Pain for more than 6 weeks
- More than 6 positive pain provocation tests in pregnancy
- Active SLR score greater than 1 in pregnancy
- Maternal age greater than 30
- Uncomfortable work posture identified on Job Content Questionnaire
- BMI greater than 25
- Depression in pregnancy
Tell Me More - The biggest recommendations the researchers give is to start monitoring pregnant women at the beginning of their pregnancies or when planning to become pregnant and give them advice on a healthy BMI. I know that you won’t often see pregnant women in PT but, if you do, you should share some information with them about their risk for this pain and PT interventions to help it. Research has shown that exercise during pregnancy decreases pelvic girdle pain, so maybe give that a mention. The authors do complain that much of the data they reviewed is heterogenous and thus tough to summarize and verify, but that they were able to get the risk factors above verified. They couldn’t do any math about pooled or combined risk due to the nature of the studies they had, jsyk.
Where dat paper at? Here
Can you predict future shoulder instability? The PRIS tool says yes.
The Gist - Over at www.margieolds.com/pris, you can see the PRIS tool, a short questionnaire that uses info about your age and dislocation along with your SPADI and TSK-11 score to predict how likely you are to redislocate next year. Recent research in JOSPT shows pretty good results, with a sensitivity of 39% and a great specificity of 95%. It correctly identified 54 of the 57 people who did not have recurrent instability. Great news!
It can’t tell you who will get it, but it’s pretty good at telling you who won’t, and that’s good in my book.
Tell Me More - The tool is a summative result of risk factors, with a bit of math popped in to get a result. They validated it through work on 85 people who had their first anterior dislocations back in 2016. They followed up at 3, 6, 9, and 12 months to collect data and used that to build the numbers above. Overall, it had a positive predictive value of 70% (but with a very wide 95% CI of 40% to 89%) and a negative predictive value of 83% (with a tight CI of 77% to 88%). That gives us a negative likelihood ratio of 0.65 and positive of 7.39. All this makes it a great tool for future predictions, though not perfect. Still, it’s definitely a step in the right direction.
I’m a stats nerd and I want more! Then you, my friend, can have it.
How do you exercise FAI? Cuz these guys think you’re doing it wrong.
The Gist - They dug through dozens of studies and extracted hundreds of exercises given for FAI to see if people were using the recommended ones and… they’re not. Due to the functional limitations of FAI (decreased single limb dynamic balance, and decreased hip flexion, adduction, and internal rotation), the researchers believe the best exercise is a single limb triplanar one that forces patients to use complex motor control strategies. According to their research, no one’s doing that. Of the 453 exercises they grabbed, only 4.6% were triplanar.
Tell Me More - If you say, well sure, not all my exercises are complicated balanced triplanar stuff, duh! Then they’re one step ahead of you. They argue that those exercises have their uses, but more should be associated with the functional limitations and demands associated with FAI. They recommend their own exercises as well, with images inside the article.
The whole article focuses on the pathomechanics of FAI, since the etiology is largely unknown and there’s no apparent causal relationship between altered biomechanics and pain. As in many areas of the body, having and FAI problem does not predict having FAI pain. They also are clear that, “there is no evidence to indicate that a more complex rehabilitation approach is associated with a greater effect,” even as they argue for the more complex exercises.
Let me at ‘em Sure thing.
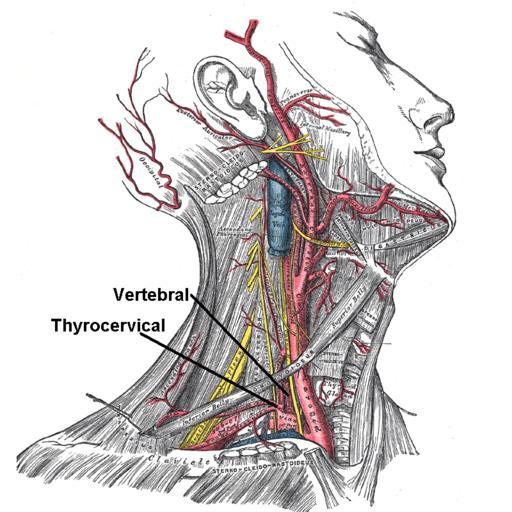
Dump vertebral artery tests? Hmmm…
The Gist - If that last article got you fired up, this one will have you jumping. In an editorial to the journal of MSK Science and Practice, these PTs argue that it’s time to dump pre-treatment positional testing of the cervical spine. They argue that major adverse events are so rare and the test so unspecific and insensitive that it’s not worth doing as the false-positive and false-negative rates are too high to bother.
They also note a few cases where the test itself caused a major adverse event, showing that it’s not perfectly safe. Beyond that, they say, a negative test can be incorrectly interpreted as safe to manipulate, even when other risk factors say you should keep your hands off.
Tell Me More - The upshot is that they want clinicians to get this at risk information through interviews and a patient history rather than from a test that they and a recent systematic review say isn’t too great at doing its job. Here’s their main argument as to what you should do:
Recently, Hutting et al. (2018) proposed three important steps in the clinical reasoning process: 1) identify a possible vasculogenic contribution or other serious pathology; 2) determine whether there is an indication or contraindication for mobilization or manipulation, and 3) assess the presence of any potential risk factors associated with a potential MAE that are reported to occur after CS mobilization and/or manipulation.
If you want all the details, it’s a well-written, short article that’s open access as well.
Show me! Here ya go. Have fun!
And that’s our week! Thanks for coming along for the ride and we’ll see you soon.
Cheers,
Luke






Comments
Want to leave a comment and discuss this with your fellow PTs? Join PT Crab and get summarized PT research in your inbox, every week.