🦀Issue 53 Blue - History, Education, Cupping, and RRI

Want the audio version of this post? Head here:

The Olympics! They’ve started, at long last. As a sports fan, this has been an incredible summer with all the events packed in. Euros, CONMEBOL cup, Nations League, Tour de France, Olympics, wow. And it seems that coronavirus has been well-controlled, in the sports at least. Keep in mind, I’m writing this a couple of weeks early, so there’s a chance that the Olympics have been canceled or something and this is all really sad, but fingers crossed that’s not the case. Is there an Olympics event you love that you think I should watch? Lmk! Shoot me an email about it. If you don’t already watch them, I highly recommend Sport Climbing (new this year), Water Polo, and the Madison in Track Cycling. Those are a few of my faves.
With that, let’s dive in!
You Can Trust Your Patient’s Subjective
The Gist - A couple of PTs from Tufts University wanted to see if patient histories were well associated with diagnoses when it came to hip pain. Good news, they were! These researchers went through dozens of articles to extract information from 9 studies that included patient history and eventual diagnosis. Through some complicated data crunching, they were able to turn self-reported info into likelihood ratios for Hip OA, making it that much easier to diagnose the condition. Don’t remember what likelihood ratios are? Check the Tell Me More section below.
Here are those ratios. Remember, they’re all for the diagnosis of Hip OA
Patients who reported a family history of hip OA had a positive LR of 2.13, family history of knee OA is an LR of 2.06, limited ROM in one or both hips is 2.87, constant low back pain or buttock pain gave a 6.50, and groin pain on the same side gave a 3.63. Considering that the classic, FABER test has a positive LR of just 1.9, these are great numbers.
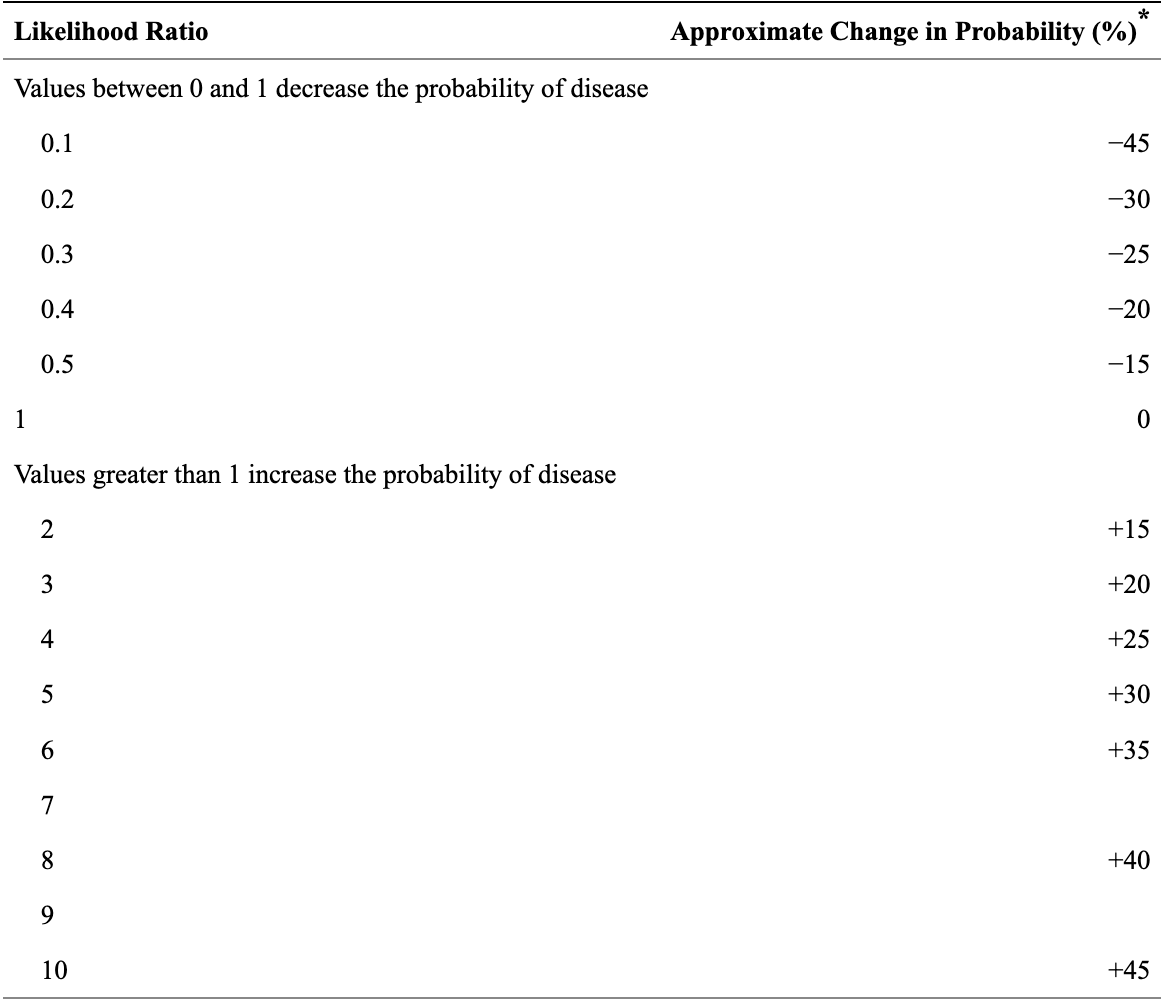
Tell Me More - So what is a likelihood ratio again? Yeah. They don’t come up too much after most people leave school. Basically, likelihood ratios increase the probability of someone having a condition. There’s a complex way of actually figuring out exact numbers by using a nomogram to compare pre and post-test probabilities but that’s just silly to use in your clinic. Instead, I offer you a much easier chart.
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1495095/table/tbl1/
So if someone has constant low back pain or buttock pain, their probability of having Hip OA increases by about 35%. That’s huge! This still relies on you having a pre-test probability in your mind before the subjective, but I’ll bet you already did anyway, didn’t you?
For more from the actual paper, there was no history obviously associated with FAI or labral pathology and only one associated with intra-articular pathology. This was crepitus, giving a positive LR of 3.56 (increasing probability by about 22%).
Overall, this paper makes a strong argument for taking a great history, so be sure your skills are on point. They say that “Multiple studies have reported that patient history alone has upward of 75% accuracy in determining patient diagnosis before performing a physical examination.” Wowza. Especially today, as telehealth becomes more common, patient histories are huge.
Can I see the paper? Sure thing boss. It’s right here.
Education + Exercise. That’s where it’s at.
The Gist - “Is patient education effective as a standalone intervention or combined with other interventions for people with knee osteoarthritis?” No! That’s the answer discovered in this systematic review from the Journal of physiotherapy. They included 29 trials with 4,107 participants that compared education only to exercise only interventions in knee OA and then checked out some combined interventions as well. Overall, they found that patient education alone was a tiny bit better than “usual care” for pain and function in the short term, but not as good as exercise. The best outcome (unsurprisingly I’d say) was a combo of patient education and exercise therapy. It was better than education alone for pain the short term and pain and function in the long term. Sweet!
Tell Me More - Does this all seem super obvious to you? Yea, it should be. Still, we need this kind of work to codify common practice in PT case. This is a relatively robust dataset, as the studies were across a huge variety of settings and many different types of patient education. That’s great for the data, but not for this newsletter, since I can’t list everything here, nor can I pull out specific examples since there’s nothing representative. So… that’s it!
Paper? Sure! It’s well written and has blow-by-blow summaries of all the included studies. And it’s open access. And it’s here.
And the highlighted version (with the most important details pointed out by me) is here.
Cupping for non-specific LBP is a specific N-O
The Gist - This RCT from the Journal of Physiotherapy grabbed 90 people with chronic, non-specific LBP to see if dry cupping was helpful. Unfortunately, it was not. Both groups had cups placed bilaterally parallel to vertebrae L1 - L5 once a week for 8 weeks. The difference was that the people in the sham group had leaky cups put on them, so the vacuum that was pulled in them released after a few seconds. After the 8 weeks, they checked their outcome measures. Primary: pain at rest, during fast walking, and during trunk flexion. Secondary: function, mobility, ROM, quality of life, psychological symptoms, and medication use.
The primary outcome (0-10 pain) grabbed a big old 0.0 difference after the first treatment and 0.6 after all 8 weeks. Confidence intervals crossed over on all the other outcome measurements, meaning that they didn’t show a large enough effect to be valuable.
Tell Me More - Here are some other bits and bobs from the study. The application period of the cups was 10 minutes at a time, once a week. The participants were blinded to their group, but the PTs weren’t, though the assessors of the data were, so that’s great. To check on the blinding efficacy at the end, the researchers asked their participants what group they thought they were in. In the experimental group, correctly 49% thought they were in that group. In the control group, 51% correctly thought they were in that group. In other words, nobody knew and everyone guessed. Probably. Across the whole study, there were three adverse events in the experimental group. One reported an increase in back pain and two others reported flu-like symptoms.
Paper? Gotcha. Open access too.
Have a running goal? You gonna get hurt.
The Gist - This survey-based study from the Dutch Consumer Safety Institute and the Department of Rehabilitation at Utrecht Medical Center wanted to see if that’s an increased chance of injury in runners who have specific performance goals. And indeed, there was. It’s not huge, but it definitely made a difference. Runners who were working up to a specific distance or running even had an odds ratio of 2.0 for injury compared with runners without a specific goal. This risk factor was half that of people with previous injuries and similar to those who were overweight. The researchers speculate that this increased injury chance is due to increased motivation to run, possibly causing them to go beyond their normal limits and leading to injury.
Tell Me More - There are many more advanced studies on training load and injury and I highly recommend scoping them out on Researchgate if you’re interested in this area of sports science and rehabilitation. This study was specifically aimed at recreational runners, your 5K types. That’s why they were able to find more information, like increased odds of injury if one runs more than 22.5hr per year. When you break it down, that’s like 25 minutes per week. Not much. That’s probably the real limitation of this study as well, it’s only applicable to more chill runners. Still, most people are chill runners, so this may be good info when you’re counseling your patients on how to get into running and avoid injury.
Paper? Of course!
That’s our week! You can become a supporter of PT Crab to get the podcast and double the articles for just $6.00 per month here.
Cheers,
Luke
