PT Crab 🦀 Issue 165 - Best of Arm, Wrist, and Elbow

We’re moving farther down the body and farther into the year with pieces on the wrist and elbow this time. And some of these are quite intense. Seriously, I’m loving this best of stuff, it’s a great refresher. I’m currently working on a more fun way to organize articles on the site, but the search function is really quite good. So if you’re looking for anything specific, pop over to PTCrab.org and search. Most older articles are for supporters only, but there’s still a lot of free stuff up there.
Before we dive into these three articles, here’s another exhortation to fill out this quick survey. Just 5 questions. Thanks to all who already have! It’s so helpful. Do it here.
And if you like all this wrist, elbow, and hand stuff, I refer you to a couple different editions that covered it in-depth. Those are Issue 127 about Lateral Epicondylalgia and Issue 113 covering Tendinopathy.
All the UE Nerves, Everywhere.
The Gist - This is going to be a long gist. You’ve been warned.
This article breaks down common injury mechanisms and diagnostic tests for upper extremity nerve injuries in throwing athletes and it really dives in. Fortunately, there are some really handy tables that you can refer to if this is a population that you regularly see. For evidence of importance of all this, a recent study showed 1.26 injuries per 1000 “athletic exposures” (e.g. games and practices) in high school baseball players. With 5 day a week practices/games for four months at this level, that’s a lot of injuries. The article has a nice breakdown of the biomechanics of overhead throwing at the beginning, so if you’re rusty on that you can give it a look as well.
For the nerves, I’ll do a quick breakdown of which they looked at and the common signs and symptoms of each.
- Suprascapular nerve
– Vague, deep posterior shoulder pain– Shoulder abduction and ER weakness– Scapular dyskinesia– Infraspinatus atrophy - Axillary nerve
– Pain and decreased sensation in lateral shoulder– “Dead arm” feeling with overhead activity– Weakness of flexion, abduction, or ER - Ulnar nerve
– Decreased throwing velocity, accuracy, or endurance– Medial elbow pain– Loss of grip strength or clumsiness in hand - Radial nerve
– Lateral elbow and dosas forearm pain worsened with resisted supination with 90 degree flexed elbow– Tenderness distal and anterior to lateral epicondyle– Weakness with finger extension - Thoracic outlet
– Vague pain, numbness, and parasthesia of throwing arm - Long thoracic nerve
– Vague shoulder pain and decreased endurance– Scapular winging - Musculocutaneous nerve
– Elbow/forearm pain– Weakness with elbow flexion– Numbness/parasthesia over dorsal forearm - Median nerve
– Vague proximal forearm or antecubital pain– Numbness in median distribution– Weakness with pronation, wrist flexion, or grip strength
Phew that was a lot. And those are just signs and symptoms from the table. Each nerve has about a paragraph that fleshes out the information above and more paragraphs on treatment. The paper also goes through the etiologies of these nerve injuries and diagnostic methods. Diagnostic methods in this paper are aimed at physicians, so you’ll see a lot of EMG/NCS and injections, but there are also physical diagnostic signs included.
If you work with upper extremity injuries at all, this paper is definitely worth a read to refresh yourself, I found it to be invaluable.
Tell Me More - How about treatment? As you may expect from a paper written by physicians, most treatment information is intended for physicians, so not super useful for physical therapy. There are some details about a PT approach, but most of them you’ll find quite obvious. Instead of going into that information, I’m going to tell you about some general considerations.
For one, the paper points out that “a Cochrane review noted very low-quality evidence with no indication of any significant neuropathic pain and symptom reduction with NSAIDs,” and that common neuropathic agents that are effective at low doses can cause lethargy and dizziness, so they should be used cautiously.
And now I’m going to sprinkle in some notes about different nerves that you may find clinically useful. For example:
- Ulnar nerve
– The traction and compressive forces at the elbow due to cocking and acceleration in throwing and the excessive valgus force combined with elbow extension all open up the nerve to injury. “Flexor carpi ulnaris contraction with the elbow flexed in the throwing motion can increase pressure in the cubital tunnel from 6 to 20 times,” and the ulnar nerve elongates 4.7mm with elbow flexion, so it’s quite exposed to hazards. - Long thoracic nerve
– “Etiology is generally an overuse traction injury with the head tilted or rotated away from the throwing arm as it is overhead.”– “Overuse long thoracic nerve injuries in throwing athletes typically spontaneously resolve with nonsurgical management in 6-18 months.” n.b. they say spontaneous, but I know physical therapists are actually fixing these folks. - MSC nerve
– “The nerve is commonly injured in the distal arm owing to overuse that includes forceful pronation of an extended elbow… more specifically, overstretching of the nerve may occur at ball release through deceleration.”
Since I’ve crossed 1,000 words, I’m going to leave this paper here for your reading pleasure. There’s a lot of great stuff in this dense paper, so I highly recommend you give it a read. The last note I have is that the authors say that many of these nerve injuries occur alongside injuries to other structures, so keep an eye out whenever you’re assessing the shoulder. K? Bye!
Paper? Gots ya.
Hand Me That Tablet, I Need To Do My Exercises
The Gist - We’ve covered ReHand before, a tablet app designed for hand exercises, and here’s a new study backing it up. In this randomized trial from the Journal of Physiotherapy, participants were given identical physical therapy treatments but different exercises. One group got a standard printout of exercises that were advanced throughout the visit cycle, while the other group was assigned tasks on ReHand, a tablet app designed for hand therapy. These were all participants with hand and/or finger bone and soft tissue injuries that limited functional abilities. They were treated 3x/wk by an OT or PT in a clinic, then prescribed their exercises at home.
The primary outcome measure was return to work and the patients with the tablets returned quite a bit faster than the others. The average time to return to work was 76 days in the experimental group and 84 in the control. This 18 day difference is 11 larger than the smallest worthwhile effect of 7, so a big difference. On secondary outcome measures of functional abilities and healthcare utilization, the experimental group spent $900 less on healthcare and scored 11 points lower on the QuickDASH. Wow.
Tell Me More - The tablet app did not sponsor the research, jsyk. Researchers reported no conflicts of interest like that. The experimental group had 20-30 minutes of exercise each day on the app and the exercises were chosen by the healthcare professionally. They’re things like pinching on the screen, moving the hand about in funny ways as directed by the app, and stretching. The tablet self-adapts to keep things within the pain-free range of the patient, which is really cool.
Since this was a collection of a lot of different injuries, let’s go through them briefly. Here are some cases that were assigned to either group.
- Fractures of radius, ulna, or scaphoid
- Fractures of one or more phalanges
- Fractures of metacarpals
- Sprains and strains
- Contusion of wrist, hand, or fingers
- Carpal tunnel syndrome
- Traumatic amputation of finger
It worked well across the variety of groups, making this an interesting option to check out for hand rehab.
I wanna learn more! Well you can. Here’s the paper.
The Big Review
The Gist - This last one is an invited topical review in the Journal of Physiotherapy from back in 2015. According to them, 40% of people will experience some form of lateral epicondylalgia in their life. Which is a lot. But where does the pain come from? They argue that it’s due to nervous sensitization since other research has shown that these people often demonstrate widespread hyperalgesia.
They recommend adding eval of the cervical and thoracic spine and neurodynamic testing of the radial nerve to see if some of the pain is coming from the spine. Neck pain appears to be more common in people with LE and presents a worse prognosis, so watch out. If you have access to diagnostic ultrasound, imaging has been shown to be helpful in diagnostics as well. Negative findings (no tears, tendon thickening, hypo echoic regions, etc.) can rule it out. A large tear (>6mm) usually fails conservative treatment.
Treatment-wise, they sum it up thusly: “exercise and load management (appear to be) the key element, with all other physical modalities being adjuncts to speed the recuperation or to enhance the effects of exercise and outcomes.”
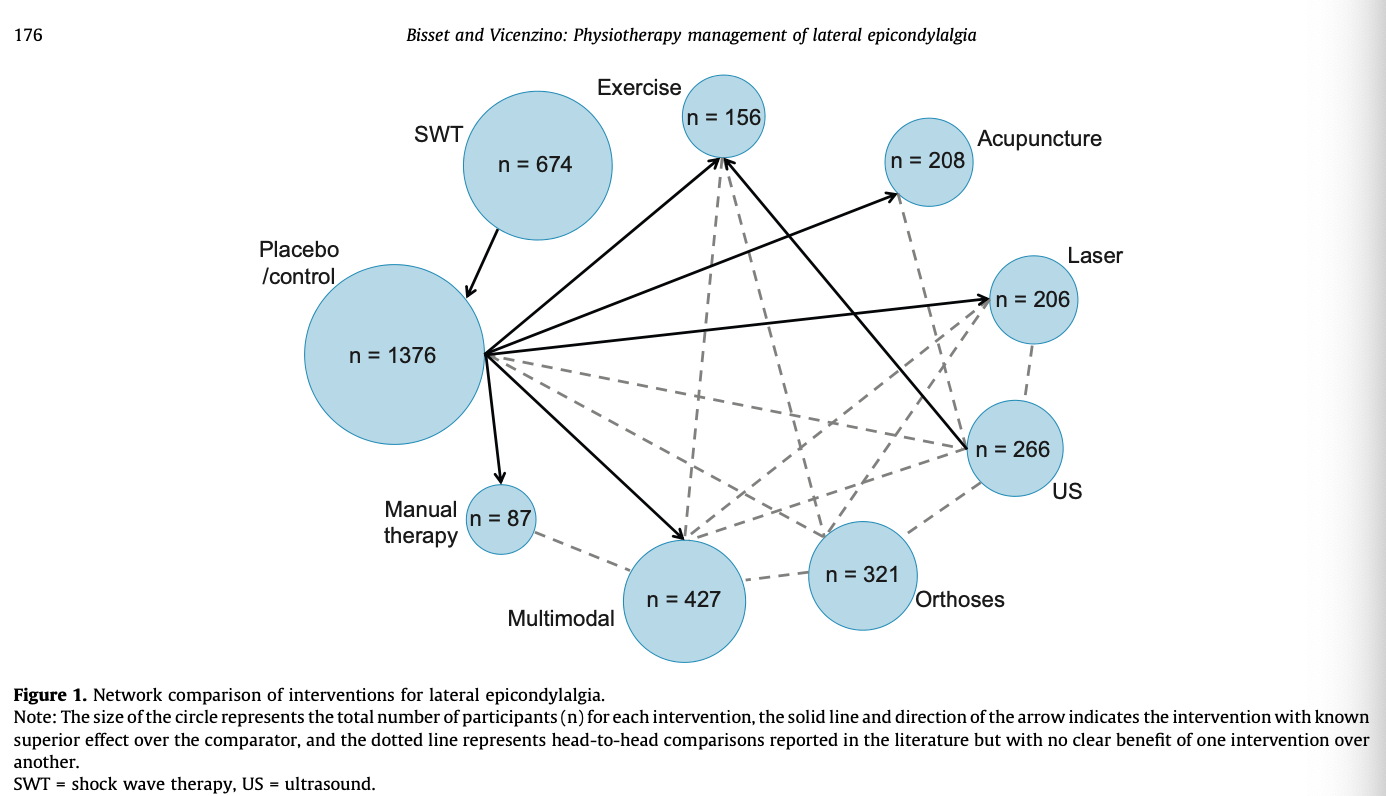
This excellent image sums up the huge amount of research that has been done on it.
Tell Me More - So what should you do? I was thinking the same thing.
“Manual therapy techniques to the elbow, wrist and cervicothoracic spine may reduce pain and increase pain-free grip strength immediately following treatment,” but we don’t know much about long-term results.
“There was conflicting evidence for the effectiveness of orthoses in providing pain relief or improvement in function compared with placebo or no treatment” though dynamic extensor orthoses combined with exercise have some effect.
On the negatives, “US appears to be no more effective than placebo for pain relief or self-perceived global improvement in the short term.” And shockwave therapy “is no more effective than placebo or other treatments for relieving pain in LE.”
And lastly, “a multimodal program of Mobilisation-with-Movement and exercise is likely superior to wait-and-see and placebo injection in the short term, and superior to corticosteroid injection in the long term. Multimodal treatment involving friction massage may be no different or worse than other treatments in providing pain relief.”
So to summarize, it seems like these three systematic reviews are telling us to tape, provide a dynamic extensor orthosis, and use mobilization with movement all along with exercise. Overall, PT does help with LE, but the details still remain fuzzy. Even those three things don’t have a ton of evidence behind them.
That’s all folks. Here’s the last paper.
Thanks again for reading! And do give the survey a shot. Please! It’s quick and will help me do better. It’s here.
Bye!






Comments
Want to leave a comment and discuss this with your fellow PTs? Join PT Crab and get summarized PT research in your inbox, every week.