🦀 PT Crab Issue 70 - Upright No.
This week, we find out the Upright Go may not be the best thing for people with PD (though it’s not useless either), that backward walking reserve speed isn’t the best measure of fall risk, what it’s like to have a hip replacement as a Physio (they’re British and thus use the better term) and what tools you should use to assess post-stroke balance (mostly). It’s half negative, half positive, and all crabby.
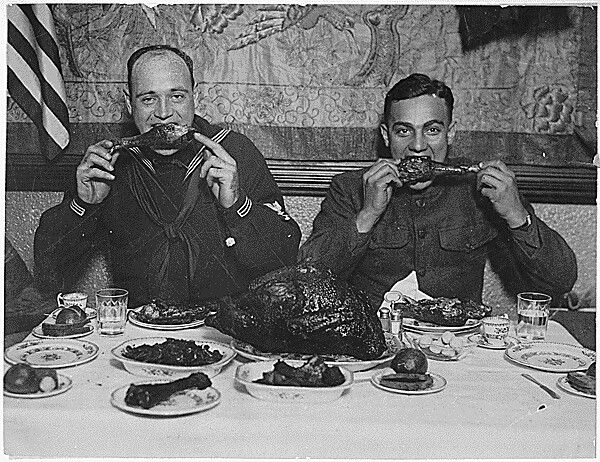
Also this week, Happy Thanksgiving! to our American readers. And Happy Thanksgiving! to everyone else too while we’re at it.
Let’s dive in!
Upright No for Parkinson’s Walking. But Sitting is Go.
The Gist - These researchers publishing in Gait and Posture dug into the effects of the Upright Go on people with moderate PD (UPDRS III: 38.5) and found some good effects and some bad ones. We’ll start good. It immediately improved neck posture in both single and dual-task environments in sitting and standing. Yay! And the benefit carried over to the 7 day span the patients spent at home. Also yay! And the bad news: gait worsened with the Upright Go. Boo! Single-task stride length, dual-task gait speed, and double support time were all significantly worse with the Upright Go. Balance was the same before and after.
To figure this all out, they placed the Upright Go on people and had them perform motor tasks “1) Sitting on a high-stool with no back with eyes open, 2) standing, feet at 10 cm apart, eyes open, looking at a poster painting, and 3) walking at comfortable speed (back and forth over 10m). Each task was 2-minutes long and repeated under single and dual-task.” They did all this while tracking metrics from multiple IMUs (inertial measurement units. Accelerometers strapped on to see what’s happenin’). They also trained the folks on how to use the device and app. After doing all this, they sent them home to use it for 7 days.
Tell Me More - If you don’t know the Upright Go, it’s a small device that either sticks or hangs on a necklace between the shoulder blades to measure posture and cue it to be better with a small vibration. It also has an app that does balance training and whatnot. I really like it because I have terrible posture and it’s quite helpful. If you’re interested, they’re at UprightPose.com and they partner with professionals (e.g. sell them cheaply to you) as well.
For this particular group, posture was indeed better, and that’s what Upright does well. But why was gait worse? Well, you’ve entered speculation territory, but it’s well-founded speculation at least. The researcher speculate that the hunched posture common to those with Parkinson’s is a compensatory posture to protect them from backwards instability. So straightening them up would lower gait confidence, hence shorter steps and lower speeds. The researchers also speculate that the vibrations from the Upright Go added an extra distraction to the gait tasks, making the participants worse at them.
Lastly, this is all about the short-term/immediate effects of the Upright Go, we don’t yet know if these effects hang around.
Paper? Sure thing boss.
Backward Walking Speed Reserve to Predict Falls. No.
The Gist - This paper from the Canadian Journal of Physiotherapy was brief and looked into whether backward walking speed reserve could predict falls better than forward walking speed. It turns out that it doesn’t, but let’s hit the details anyway. It’s quite interesting. First off, backward walking speed reserve is the difference between maximal walking speed and self-selected walking speed, so they got these by measuring both across a GaitRite measurement device. The participants were half healthy older people and half older adults who have been identified as a fall risk, all without assistive devices.
Basically, the math they did was compare the reserve speeds between the two groups to see if there was a trend that stood out between the fall risk and the not fall risk folks. Unfortunately for their hypothesis, there was not. Rather, they reconfirmed that self-selected walking speed is the best predictor we have right now.
Tell Me More - The only more left in this short, four page study is some interesting detail about muscles and whatnot from the end. So I’m going to block quote it a bit here
It has been shown that during backward walking in young adults, the ankle joint primarily contributes to propulsion and shock absorption rather than the knee and hip joints. Whether this is true for older adults needs to be examined. Older adults have been shown to have altered joint mechanics, with increased use of hip extensors and reduced use of plantar flexors during forward walking compared with younger adults. Future studies should assess whether these altered mechanics or reduced strength among older adults contributes to their inability to increase backward maximal walking speed.
And that’s all she (okay, they) wrote.
Paper? Oh, Canada yet again.
What Are The Best Quantitative Tools for Assessing Static and Dynamic Standing Balance after Stroke?
The Gist - Wouldn’t it be nice if we had a paper with this very title? Wait, we do? Wow, how convenient. It’s like one of those movies where the same writer gets to choose what both sides of an argument would say leading to a surprising and wonderful conclusion sigh. Wait, where was I?
This systematic review wanted to answer my question above, so they did lotsa number crunching. If you’re interested in this field, you should give the whole thing a go since the details are definitely not summarizable (that’s like the definition of details…). The overview is that they checked generalizability, reliability, and construct validity as well as clinical utility (with a really cool, validated scoring system) to see which analyses were best. 22 studies with 773 people were included and the winners were the Five Step Test and the Sideways Step Test but many worked rather well, including the Turn test and Quiet Standing Test on a Force Platform. And if this doesn’t seem like enough information well I already warned you it wouldn’t be so just read the paper okay?
Tell Me More - Before you go read the paper (which you obviously will now), you should know a few more details. For one, the clinical utility score for all tests overall was 7 out of 10, 9 being their cutoff for really useful. 7 of them did get 9 or more, which was great. These were the “five-step test, side-step test, sideways step test, step length, timed 180° turn test, and timed 360° turn test.” To close out, I’m going to dig into this clinical utility scale a bit more. It’s based on a review by Tyson and Connell in the Journal of Clinical Rehabilitation and takes into account the amount of time needed to complete the test, the cost of equipment, the amount of training needed, and how portable it is. It’s quite a swell list and should be used by more authors. I’m obviously a fan. Now, I implore you that if you want information from this one enough to actually use the data, give the whole paper a look. Don’t get bogged down in the analysis and criteria and whatnot, but do read through the assessments to understand how to use them. Bye!
Paper? God, I thought you’d never ask.
A Physio’s Total Hip
The Gist - This perspective piece from the British Journal of Sports Medicine is brought to us by Louise Grant, a hip specialist who needed one of her own. She tore her labrum in 2011, requiring arthroscopy, then took a catastrophic fall while slightly drunk and wearing heels on her birthday that broke her elbow, tore up her wrist, and decapitated her left hip. So it was time for a new one. Just because she’d been rehabbing them for thirty years didn’t mean she wasn’t nervous,
I have watched many hip operations over the years, so I knew full well what would happen in the operation... saws, hammers and bits of me moving in ways you don’t want to think about… On my surgery day… past patient’s faces who have had some of those things happen to them came into my mind like the ‘Ghosts of Christmas Past’. I tried my best to block these visions out.
She used her experience to start a new organization and website to guide THR patients into their surgeries and through their rehab and says that the most important thing to her after surgery was the tight communication between her surgical and rehab team and her intentionally tortoise-like path through rehab. If you want to read a nice, succinct patient voice piece, give this one a look.
Paper? Yupp yupp yupp.
And that’s our week! Please do share with friends, Facebook groups, enemies, the lot. Every little helps.
Happy Thanksgiving!
Here are the articles we covered this week:
Bruyneel, A.-V., & Dubé, F. (2021). Best Quantitative Tools for Assessing Static and Dynamic Standing Balance after Stroke: A Systematic Review. Physiotherapy Canada, 73(4), 329–340. https://doi.org/10.3138/ptc-2020-0005
Grant, L. (2020). My total hip replacement. British Journal of Sports Medicine. https://doi.org/10.1136/bjsports-2019-101899
Stuart, S., Godfrey, A., & Mancini, M. (2022). Staying UpRight in Parkinson’s disease: A pilot study of a novel wearable postural intervention. Gait & Posture, 91, 86–93. https://doi.org/10.1016/j.gaitpost.2021.09.202
Yada, T. T., Taulbee, L., Balasubramanian, C., Freund, J., & Vallabhajosula, S. (2021). Can Backward Walking Speed Reserve Discriminate Older Adults at High Fall Risk? Physiotherapy Canada, 73(4), 353–357. https://doi.org/10.3138/ptc-2019-0086






Comments
Want to leave a comment and discuss this with your fellow PTs? Join PT Crab and get summarized PT research in your inbox, every week.